What Can Be Done About Meniscal Tear?

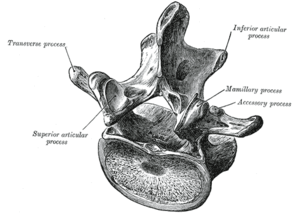
Image via Wikipedia
The meniscus is a shallow bowl shaped piece of cartilage that is attached to the lower leg bone, or tibia. There is a medial meniscus (inner half of knee) and a lateral meniscus (outer half of knee).
The end of the femur (upper leg) bone has two protuberances called the femoral condyles, which rest on top of the meniscii (plural). In the standing position, the meniscii bear the full weight of the body above the knee. They serve as a cushion and shock absorber and protect both of the ends of the tibia and the femur. The meniscus also guide the action of the femoral condyles as you bend and extend your knee.
The knee is obviously a highly utilized, weight bearing joint. It has the largest suface contact area of any joint in the body as it has to bear most of the body’s weight and on top of that, absorb shock from walking, running and jumping. It is held together by several strong ligaments, the primary being the anterior and posterior cruciate ligaments (ACL, PCL), the medial and lateral collateral ligaments (MCL, LCL), and the patellar tendons. It is a synovial joint, which means it is totally encapsulated and lined with synovium, a specialized tissue that secretes synovial fluid to lubricate the joint.
The slightest alteration in the inner workings of the knee will lead to problems. A common one is a meniscal tear. The two basic types are a radial meniscal tear and a vertical meniscal tear. A radial tear that expands forms what is called a “bucket handle” tear (3rd set in the below image- top and bottom).

Meniscal tears are caused by excessive pounding forces to the knee, which weaken the meniscii over time. Eventually a tiny tear forms, which grows in length as the individual continues to engage in the offensive activity (running on hard pavement, weight lifting, playing basketball, etc.), much like how a tiny crack in a car windshield grows into a long crack over time . If a small piece breaks free, it floats inside the knee space, suspended in the synovial fluid. Like a grain of sand in a watch, it interferes with the moving parts and can cause the knee to swell and become stiff.. Pain is felt deep inside the knee and is worse with prolonged standing and transitioning from sitting to standing.
Meniscal tears increase the chances of accelerated knee osteoarthritis, as “bone on bone” contact occurs between the ends of the femur and tibia.
TREATMENT: Diagnosis is made with a knee MRI and arthroscopy. Meniscal tears will most likely require arthroscopic surgery involving repair to the tear. If you have a gradual onset of deep, focal knee pain accompanied by knee stiffness that doesn’t go away, see your doctor.
Prevention, as always, is the key. I advise against sports that involve consistent and prolonged pounding forces to the knee. This includes long distance running and frequent hard court basketball that involves jumping. Consider doing functional exercises that combine cardio and strength instead.
Most leg exercises will strengthen the knee. Do mostly closed kinetic chain exercises where the foot is immobilized. This includes squats and lunges.
Intermittent jumping exercises are ok as long as they are controlled and are not the focus of an exercise session. Power jumps and related plyometric exercises fall into this category.
Most meniscal tears grow too large to heal on their own by the time the patient seeks medical help. This is why surgery is the only option. The surgeon stitches together the tear, but thanks to the forces the knee has to endure, the tear often returns.
Some patients do not get surgery, and let the tear become chronic. When it’s chronic, there is less acute pain, and more of a broad, dull pain in the knee. In this scenario, the knee joint will experience accelerated degeneration, leading to knee osteoarthritis. Eventually in the later years, knee replacement surgery is needed.
I made a general Knee Pain Rehab instruction video that includes things one can do to help deal with early stage knee pain.