The Origins of Musculoskeletal Pain – Which Describes Yours?
Musculoskeletal pain refers to pain affecting the muscles, ligaments, tendons, joints and sometimes bones. Sometimes it is straight-forward; other times it is not. Before you convince yourself that you know the origin/cause of your musculoskeletal pain, consider the following:
Pain can be due to trauma/injury where the tissue itself is generating the pain due to ruptured cells and the effects of inflammation. This is the most unambiguous case because it is connected to an identifiable event. This pain can be acute, meaning relatively recent onset; sub-acute, referring to a state where the injury still is healing but pain and some swelling is still present; and chronic, which basically means symptoms that remain after the body has done all it can at the moment to heal the injury.
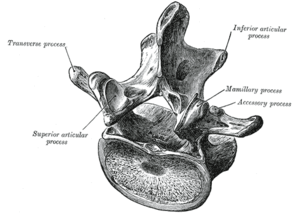
Pain can manifest in one area of your body due to abnormal movement in a distal location. The abnormal movement might be caused by a previous trauma event like a car accident or sports injury, it can be congenital (developed at birth) and it can be from repetitive movements required by a certain occupation or hobby/sport. Abnormal movement (called dyskinesia) can also arise from muscle imbalances, where one muscle loses strength due to inactivity, decreasing joint stability and facilitating excessive, restricted, or other abnormal movement of that joint, forcing distal joints to make up the difference in lost movement or compensate to create more stabilization. The distal muscle(s)/joint(s) then work in a fashion that they were not designed for, leading to strain, spasm and even injury to the muscle or joint.
This is the most tricky type of pain manifestation because it is often mis-diagnosed resulting in the wrong treatment approach and lack of resolution. An example of this is sciatica (pain in the buttock) from a spasmed piriformis muscle scissoring the sciatic nerve due to an unlevel pelvis coming from hyperactive same-side erector spinae musculature. If the back muscle and pelvic imbalance is not corrected and the patient simply gets massage to the piriformis muscle, you can see how this pain will never go away with this type of treatment.
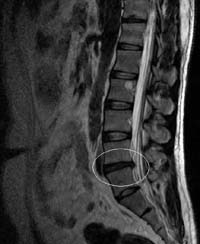
Pain can be referred pain. In referred pain, the brain senses the pain to be in one area of the body when the abnormal site is actually in another area. Despite an increasing amount of literature on the subject, the mechanism of referred pain is still unknown. Going back to the heart attack example, myocardial infarction can cause referred pain to the left jaw and left arm. The image below illustrates commonly observed types of referred pain and their true source (credit to Wikipedia).
Pain can arise from hypoxia (insufficient oxygen to the tissues). An extreme example of this kind of pain is a myocardial infarction, or “heart attack” where a major artery to the heart muscle is blocked, preventing oxygen from reaching a section of the heart. Biochemical reactions take place when this happens, which generate pain.
Thoracic outlet syndrome is a condition where the nerves and blood vessels supplying the arm get compressed in the neck region by tight scalene muscles or the collar bone. The resulting hypoxia can contribute to pain in the arms and hands.
Pain can come from trigger points, also known as trigger sites or muscle knots, are described as “hyper-irritable spots in skeletal muscle that are associated with palpable nodules in taut bands of muscle fibers.” Trigger points are usually only a few centimeters in diameter.
Clinical textbooks on the subject establish the following requirements to meet the definition of trigger points:
- Pain related to a discrete, irritable point in skeletal muscle or fascia, not caused by acute local trauma, inflammation, degeneration, neoplasm or infection.
- The painful point can be felt as a nodule or band in the muscle, and a twitch response can be elicited on stimulation of the trigger point.
- Palpation of the trigger point reproduces the patient’s complaint of pain, and the pain radiates in a distribution typical of the specific muscle harboring the trigger point.
- The pain cannot be explained by findings on neurological examination.
As in referred pain, the mechanism of trigger points is still being debated. Trigger point tissues have been biopsied, and findings indicate the presence of hyperactive muscle spindles, special cells whose function is to detect the rate of lengthening in a contracting skeletal muscle and initiating the firing of complementary muscles to complete the desired goal.
Wikipedia gives a nice summary of what causes trigger points to form:
Activation of trigger points may be caused by a number of factors, including acute or chronic muscle overload, activation by other trigger points (key/satellite, primary/secondary), disease, psychological distress (via systemic inflammation), homeostatic imbalances, direct trauma to the region, collision trauma (such as a car crash which stresses many muscles and causes instant trigger points) radiculopathy, infections and health issues such as smoking.
Finally, there are more highly-complex causes of pain related to dysfunction of the central nervous system, sympathetic nerves, biochemical and hormonal issues, and even psychosomatic. These types of cases are difficult to diagnose and are often treated using pharmacological agents, and on the other side of the spectrum, holistic approaches with mixed results.
NO MATTER what pain you may be experiencing, know that it always, always helps to detoxify your body as best you can via a nutritionally-dense diet centered on naturally-occurring, non-GMO, organic unprocessed food sources; reducing your processed sugar and grain intake; regular exercise, getting enough sunshine to your body; targeted supplementation, meditation or other relaxation methods, and even nurturing social support. This is the theme of this blog, because there is no shortage of treatment methods for pain and not enough emphasis coming from doctors or the government on prevention, wellness and health optimization; i.e. Healthy Lifestyle Education.
In the next couple of blog posts, I will talk about real, practical ways you can reduce your pain without the help of your doctor by making strategic lifestyle modifications. Your body has a potent array of disease-fighting systems and has an innate ability to repair and regenerate itself. The problem is that in many pain sufferers, these systems are burdened by unhealthy habits and are not running at their full potential. Imagine what can happen if those systems were brought back on line, constantly doing what they are naturally programmed to do– protect you and keep you alive; fighting germs, cancer cells and developing diseases; and repairing injured sites so that you can function better. Isn’t this a goal worthy of your efforts?
More to come, stay tuned!
Dr. Perez


 Whole body vibration, or WBV is popular in the fitness, health, and beauty industries. It involves standing stationary or doing exercises on a motorized platform that vibrates at different frequencies and amplitudes (basically, different speeds and intensities).
Whole body vibration, or WBV is popular in the fitness, health, and beauty industries. It involves standing stationary or doing exercises on a motorized platform that vibrates at different frequencies and amplitudes (basically, different speeds and intensities).