How to manage lower back strain
Low back pain is said to be the most common cause of lost work days, after the common cold. Most everyone has experienced an episode of lower back pain at some point in their life; millions suffer from chronic (ongoing; unending) lower back pain of some form.
The low back, or lumbar spine, is comprised of the last five (5) vertebrae in the spine. These vertebrae are the largest as they support most of the body’s torso weight. Like the cervical spine; i.e. neck (the first 7 bones of the spine), there are no rib attachments in the lumbar spine to limit movement, making the lumbar spine more moveable than the thoracic spine (torso), but less flexible than the cervical spine due to its larger, heavier vertebrae.
This unique lumbar spine design offers advantages and disadvantges. The obvious advantage is flexibility–you can bend (flex) your low back forward, backward, sideways, and can rotate it a few degrees to either side. The disadvantage is that with more movement, there are more opportunities to stress the joints of the lumbar spine (more moving parts) and therefore more chance of injury and pain. This includes potential injury/ trauma to the surrounding ligaments, joint capsules, cartilage lining the small joint surfaces; small facet joints, intervertebral discs, and the lumbar vertebrae themselves.
Therefore, low back pain can originate in one of several structures in the lower back:
- the discs (strong fibro-cartilage ligaments that hold vertebrae together)
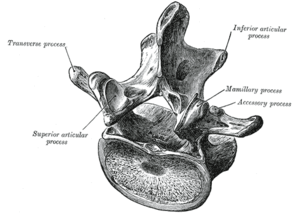
- the facet joints (the “rear” joints of a vertebra, opposite the vertebral

Image via Wikipedia
bodies)
- the pars– the small extensions of bone to either side of the vertebrae that form the upper and lower borders of the intervertebral foramen, and end in the lumbar facet joints
- the surrounding muscles
- the surrounding fascia (muscle covering)
- the nerve roots inside the spinal canal
- the vertebrae itself (compression fractures; vertebral end-plate fractures)
Today we’ll address lower back pain due to muscle and fascia strain. I’ll refer to this a low back or lumbar strain. This is a common cause of lower back pain and is more manageable than pain due to deeper spinal structures.
In the many cases of lower back strain that I’ve treated over the years, the patient describes a sudden onset of pain after bending at the waist reaching for something. In other cases, the pain starts a day after doing something like weight lifting, running or rock climbing.
Medically speaking, a muscle sprain-strain occurs when muscle fibers tear during contraction and subsequently release inflammation.
The convention for naming soft tissue injuries is that strain refers to injury to a muscle and tendon while sprain refers to injury to ligaments, which connect bone to bone. Since muscles, ligaments and tendons typically get injured all at once in a typical injury due to their anatomical proximity to one another, doctors refer to these types of injuries as sprain-strain injuries.
Sprain-strain severity is described as Grade I, Grade II and Grade III, with Grade III being the most severe and refers to complete rupture of a tendon or ligament. Most lumbar strains are Grade I and II.
Inflammation is meant to contain/ quarantine an injury and is actually an important process in the healing phase (tissue regeneration). The problem is that it releases chemicals that irritate nerves and surrounding tissues, and stiffens adjacent muscles and joints. The inflammatory response can “overshoot” causing the patient to needlessly suffer.
If you go to your doctor complaining of lower back strain, and tests do not indicate damage to deeper structures (discs, facet joints, nerve roots, bone) then you will most likely be prescribed pain blockers (usually NSAIDs- non-steroidal anti-inflammatories), rest, and ice. Your doctor will likely put you on “temporary disability” which means no heavy lifting, bending at the waist, and other activities that put stress on the lower back. Sometimes muscle relaxants are prescribed, if there are complaints of spasm and stiffness. You will be told that it should resolve on its own, and most cases do.
TREATMENT:
At first onset of straining your back, apply ice for 20 minutes every two hours of the waking day. The easiest way in my opinion is to get a large freezer ziplock back, fill a third of it with ice cubes, put about a cup of water in the back and zip it closed (get as much air out as possible before closing shut).
Lie down so that your exposed (no clothing) lower back is directly on top of the bag. Bend your knees or put a pillow under them for comfort. This flattens the lower back and allows it to make good contact with the icepack. (Optional: put a neck roll under your neck for comfort). Do this for 1-2 days.
On the second day, you can introduce gentle stretches while you ice. After your 20 minutes of icing, try lifting your knees to your chest, pulling them gently towards you with your hands. Hold for 5 seconds; repeat five times. Then, keeping your feet together (you are still lying on your back), knees bent, let the knees fall to the right side, gently twisting the lower back; reverse sides. Do five times to each side. What these movements do is orient any scar tissue that develops, in the direction of contraction.
On the third day, assuming pain is still present, you can try using heat. I recommend an infrared lamp. This is radiant heat that penetrates deeper than a hotpack.
If you need to get pain free even sooner, I suggest using the 120 LED (Light Emitting Diode) wrap. This popular home therapy device used red light therapy + infrared heat, which goes beyond simply blood circulation increase. The red light diodes inhibit inflammation and increase cellular metabolism (energy production, waste removal) which means speedier tissue healing.
After a week, your lower back strain should be 60-90% better. If it is only 25% or so improved after a week, the injury is likely worse than originally thought; and deeper soft tissues may be involved. In this case, consider using Pulsed EMF to further enhance tissue healing.
Last thought: I believe that if someone strains his lower back by simply bending forward, it indicates that the back muscles, and probably core/abdominal muscles need better conditioning. It’s not all about strength, it’s also muscle coordination in response to varying loads; for example, picking up a piece of heavy luggage. Those with excellent muscle coordination (there are five major muscle groups that have to work together to move the lower back) are less likely to injure their backs like this. Interestingly, research shows that osteoarthritis, or degenerative joint disease in the lumbar spine, is related to poor lower back muscle coordination. And it makes sense– your muscles move and support your lumbar spine. Poor support and coordination between muscles (erector spinae group, abdominals, etc.) can cause your spinal joints to bear more stress than normal during every day movements.
So, the best strategy is to prevent getting lower back strain by strengthening AND conditioning (improve coordination of) your lower back muscles by doing functional exercises.